Chronic migraines affect millions, causing debilitating pain that disrupts daily life. Traditional treatments often fall short, leaving many sufferers searching for effective alternatives.
Ketamine, historically known as an anesthetic, is emerging as a potential solution for migraine relief. This intriguing option works by blocking pain signals in the brain, offering hope to those who have not found relief through conventional methods. As interest in ketamine therapy grows, it raises the question: could this be the breakthrough chronic migraine sufferers have been waiting for? Could ketamine be the answer to chronic migraine relief?
Understanding Chronic Migraines
Chronic migraines are a debilitating condition that significantly impacts the lives of millions worldwide. Defined by the presence of headaches occurring on 15 or more days per month, with at least eight of these being migraines, this condition extends beyond occasional discomfort, often causing severe disruptions in daily life.
Unlike episodic migraines, chronic migraines can persist over long periods, leading to physical, emotional, and social challenges for those affected.
Description of Chronic Migraines
Chronic migraines differ from regular headaches in both intensity and frequency. These migraines often involve severe, pulsating pain that typically affects one side of the head. Accompanying symptoms may include sensitivity to light and sound, nausea, and visual disturbances such as auras.
For many sufferers, the pain and related symptoms are so severe that they disrupt work, relationships, and daily responsibilities. This condition is also associated with a heightened risk of anxiety and depression, compounding the overall burden on a person’s mental health.
Chronic migraines are more than just a headache; they represent a complex neurological condition. Some of the most common symptoms include:
- Intense Headache: Throbbing pain, usually localized to one side of the head, can persist for hours or even days.
- Sensitivity to Light and Sound: Exposure to bright lights or loud noises can exacerbate symptoms, making it difficult for patients to function in normal environments.
- Nausea and Vomiting: Many individuals experience gastrointestinal symptoms, further limiting their ability to eat or drink comfortably.
- Cognitive Impairment: Brain fog, difficulty concentrating, and fatigue are frequent complaints during and between migraine episodes.



Overview of Traditional Treatments
Traditional treatments for chronic migraines include a combination of medications, lifestyle changes, and preventive strategies. Medications such as triptans, beta-blockers, anti-seizure drugs, and antidepressants are commonly prescribed.
Botox injections and CGRP inhibitors have also gained traction in recent years. Alongside pharmaceutical approaches, lifestyle changes like maintaining a consistent sleep schedule, reducing stress, avoiding triggers, and regular exercise are often recommended.
While these treatments can provide relief for some patients, they are not universally effective. Many patients still struggle with breakthrough migraines despite adhering to their prescribed regimen. These individuals, often referred to as having refractory migraines, face persistent challenges.
Limitations and Challenges Faced by Patients with Refractory Migraines
For patients with refractory migraines, traditional treatments often fall short. They may experience incomplete relief or intolerable side effects from medications. The unpredictability and intensity of migraines can lead to frequent absences from work or school and hinder social interactions, leading to isolation.
Moreover, the stigma surrounding chronic migraines can discourage individuals from seeking help or adhering to treatment plans. This gap in effective care has spurred the exploration of alternative treatments, including the use of ketamine.
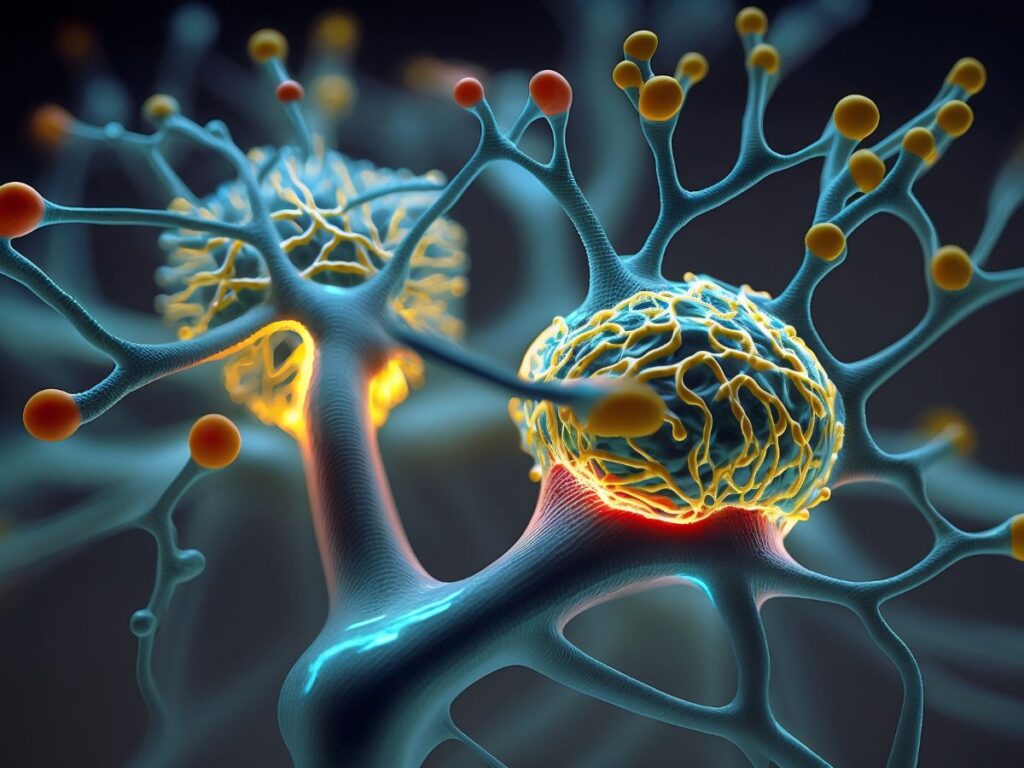
How Ketamine Works on NMDA Receptors
Ketamine is a dissociative anesthetic that has gained attention for its novel approach to pain management. Its primary mechanism of action involves blocking N-methyl-D-aspartate (NMDA) receptors in the brain. These receptors play a critical role in transmitting pain signals and are involved in the processes that amplify chronic pain. By inhibiting NMDA receptor activity, ketamine can reduce the hypersensitivity of the nervous system, offering relief to individuals with chronic migraines.
Ketamine's effect on NMDA receptors also extends to its ability to modulate glutamate, a neurotransmitter implicated in both pain perception and mood regulation. This dual action may contribute to its effectiveness in reducing the frequency and intensity of migraines while also addressing the emotional distress often associated with chronic pain.
Benefits and Risks of Ketamine Treatment
Ketamine has emerged as a promising treatment for various medical conditions, from chronic pain to severe depression and, more recently, refractory migraines. Its unique mechanism of action sets it apart from traditional therapies, offering hope to patients who have not responded to conventional treatments. However, as with any medical intervention, ketamine treatment comes with both potential benefits and risks that must be carefully weighed.
Potential Benefits
One of ketamine’s most significant advantages lies in its rapid onset of action. Unlike many medications that require weeks to show results, ketamine can provide relief within hours or days. For individuals experiencing debilitating pain or depression, this quick response can be life-changing.
- Pain Relief: Ketamine’s ability to block N-methyl-D-aspartate (NMDA) receptors helps reduce chronic pain by disrupting pain pathways in the brain. This makes it a valuable option for conditions like refractory migraines, fibromyalgia, and complex regional pain syndrome.
- Mood Improvement: By modulating glutamate, ketamine positively influences mood and emotional regulation. This is particularly beneficial for patients with co-existing depression or anxiety, conditions that often accompany chronic pain disorders.
- Neuroplasticity Enhancement: Research suggests that ketamine promotes neuroplasticity, the brain’s ability to form new neural connections. This can help reset dysfunctional pain and mood pathways, leading to longer-term improvements even after treatment ends.
- Treatment-Resistant Conditions: Ketamine has shown promise in treating conditions that have not responded to standard therapies. For patients with refractory migraines or treatment-resistant depression, it offers a new pathway to relief.
- Improved Quality of Life: By alleviating both physical and emotional symptoms, ketamine can significantly enhance a patient’s overall well-being, enabling them to return to daily activities and social interactions.




Possible Side Effects
While ketamine offers substantial benefits, it is not without risks. Understanding potential side effects is crucial for ensuring its safe and effective use.
- Dissociative Effects: Ketamine’s dissociative properties, while therapeutic in some contexts, can cause temporary feelings of detachment from reality, hallucinations, or a sense of being outside one’s body. These effects typically resolve shortly after treatment.
- Nausea and Vomiting: Some patients may experience gastrointestinal discomfort during or after the administration of ketamine.
- Cardiovascular Effects: Ketamine can temporarily elevate blood pressure and heart rate, which may pose risks for individuals with certain cardiovascular conditions.
- Cognitive Impairment: Short-term confusion, memory lapses, or difficulty concentrating may occur, though these effects usually subside within hours.
- Addiction Potential: Although rare in clinical settings, ketamine has a history of recreational misuse. Strict medical supervision minimizes this risk.
- Bladder Issues: Prolonged or repeated high-dose use has been associated with urinary tract and bladder problems, though these are uncommon in controlled therapeutic use.




Clinical Considerations for Ketamine for Chronic Migraine
Effective ketamine treatment requires careful planning and ongoing oversight. Proper patient selection, tailored dosing, and thorough monitoring are essential to maximize benefits and minimize risks.
Patient Selection Criteria
Not everyone is a suitable candidate for ketamine therapy. Clinicians must evaluate patients on an individual basis, considering their medical history, current conditions, and treatment goals.
- Refractory Conditions: Ketamine is often reserved for patients who have not responded to traditional treatments. This includes those with refractory migraines, treatment-resistant depression, or chronic pain disorders.
- Mental Health Screening: Since ketamine can induce dissociative states, patients with certain psychiatric conditions, such as active psychosis or untreated bipolar disorder, may not be ideal candidates.
- Physical Health Evaluation: Patients with uncontrolled hypertension, severe cardiovascular disease, or liver dysfunction may require additional precautions or alternative treatments.
- Commitment to Treatment: Because ketamine often requires multiple sessions and follow-up care, patients must be willing and able to adhere to the treatment plan.
Monitoring and Follow-Up
The administration of ketamine requires close monitoring during and after treatment to ensure patient safety and optimize outcomes.
- Initial Monitoring: Ketamine is typically administered in a controlled medical setting under the supervision of trained professionals. Vital signs such as blood pressure, heart rate, and oxygen levels are closely monitored during the infusion or injection.
- Managing Side Effects: Clinicians are prepared to address common side effects, such as nausea or dissociation, during treatment. Supportive care ensures patients feel safe and comfortable throughout the process.
- Post-Treatment Assessment: After the initial treatment session, patients are observed for any lingering side effects or adverse reactions. Follow-up assessments allow clinicians to gauge the treatment’s effectiveness and make any necessary adjustments.
- Ongoing Care: Ketamine is often part of a comprehensive treatment plan that includes other therapies, such as counseling, physical therapy, or additional medications. Regular follow-up appointments help track progress and address any new or persistent symptoms.
- Safety Measures: To reduce the risk of misuse, ketamine is administered only in medical settings, and patients are educated about the importance of adhering to prescribed doses and schedules.
Ketamine for Chronic Pain Management
Ketamine presents a promising avenue for chronic pain management, particularly for those grappling with debilitating migraines. Its unique mechanism of action offers hope where traditional treatments may have failed.
As research continues and more patients share their experiences, ketamine could redefine the landscape of migraine relief. If you or someone you know struggles with chronic pain, exploring ketamine therapy may be a worthwhile consideration. Stay informed and consult with healthcare professionals to determine the best path forward for your pain management journey.
