Ketamine therapy has emerged as a new frontier for people struggling with depression, post-traumatic stress disorder (PTSD), chronic pain, and treatment-resistant anxiety. It offers hope when traditional medications stop working or never work at all. Yet, not everyone is a candidate for it.
What disqualifies you from ketamine therapy is not just one thing but a combination of medical, psychological, and lifestyle factors that determine whether the treatment is safe and effective for you. Understanding these disqualifiers helps ensure that patients receive care tailored to their bodies, histories, and emotional needs while minimizing risks and maximizing benefits.
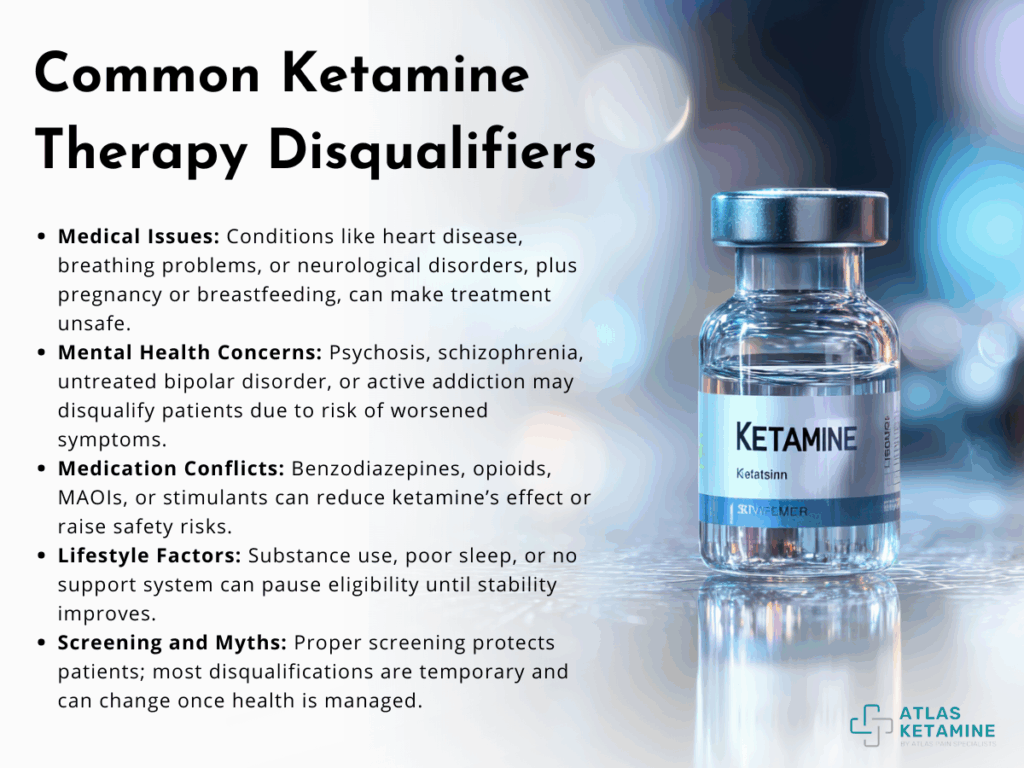
1. Medical Conditions That Can Make Ketamine Unsafe
Before considering ketamine therapy, every patient undergoes a thorough medical evaluation. The purpose is to uncover any conditions that could cause complications once the treatment begins. Ketamine alters heart rate, blood pressure, and brain activity, meaning certain medical backgrounds can pose real risks.
The most common medical disqualifiers are uncontrolled heart conditions, severe respiratory issues, and certain neurological disorders.
People with a history of uncontrolled hypertension or heart disease are often advised against ketamine therapy because the drug can raise blood pressure temporarily. This isn’t usually dangerous for healthy individuals, but it may trigger complications like arrhythmias or chest pain in those with cardiovascular problems. Similarly, individuals with severe chronic obstructive pulmonary disease (COPD) or other respiratory limitations may struggle because ketamine can depress breathing in high doses.


Neurological concerns are another area of caution. Patients with a history of brain injury, epilepsy, or elevated intracranial pressure need special assessment before proceeding. Ketamine changes cerebral blood flow and pressure, so these conditions may worsen during infusion. Those with liver or kidney disease may also be at risk since the body’s ability to process the drug can be impaired.
Finally, pregnancy and breastfeeding generally disqualify individuals from ketamine therapy. There’s not enough scientific data confirming its safety for developing babies or infants, so most clinics err on the side of caution and delay treatment until after pregnancy or lactation.


In short, while ketamine can be transformative, its effects on circulation, breathing, and the brain mean it should only be used when the body can handle it safely.
2. Mental Health Histories That Require Caution
Ketamine therapy is a mental health treatment at its core. It can relieve emotional pain, dissolve intrusive thoughts, and spark new neural connections that restore hope. However, some mental health conditions may disqualify a person from ketamine therapy because the altered state it produces can worsen certain symptoms or create new risks.
People with a history of psychosis or schizophrenia are generally not good candidates. Ketamine temporarily induces dissociation,a sense of detachment from reality, which can trigger hallucinations or delusions in individuals with these disorders.


Similarly, those with untreated bipolar disorder may experience manic or hypomanic episodes following ketamine administration. Clinics typically ensure a patient’s mood is stabilized with other medications before considering infusion.
Substance use history also plays a key role. Because ketamine itself has abuse potential, individuals with active addiction or recent substance misuse may be disqualified. This doesn’t mean people in recovery are automatically excluded; many clinics accept patients who have maintained sobriety and have ongoing support systems such as therapy or recovery programs. The goal is to ensure that ketamine becomes a healing tool, not a relapse trigger.
Patients who struggle with borderline personality disorder or severe dissociative disorders may also require cautious evaluation. Since ketamine temporarily alters perception and emotional boundaries, it could intensify instability or self-harm urges if not carefully monitored.

To put it simply, mental health conditions that affect perception, impulse control, or reality testing require the highest level of screening and supervision. When used responsibly, ketamine can help rewire the brain. But without careful assessment, it can disrupt fragile psychological balance instead of restoring it.
3. Medication and Drug Interactions
Even when a person’s medical and psychological health align well with ketamine therapy, certain drug interactions can change that equation. Many individuals seeking ketamine treatment already take antidepressants, pain medications, or sleep aids. While some combinations are safe, others interfere with ketamine’s mechanisms or raise safety concerns.
The most common medication-related disqualifiers include benzodiazepines, high-dose opioids, and certain blood pressure or thyroid medications.
Benzodiazepines like Xanax, Valium, or Ativan can blunt ketamine’s antidepressant effects because they act on similar neurotransmitters but in opposing ways. High doses of these medications reduce the likelihood that patients will experience the full benefit of ketamine’s mood-lifting properties.

In some clinics, patients are asked to taper down under medical supervision before starting infusion sessions.Opioid use introduces another complication. Both opioids and ketamine act on NMDA receptors, and when taken together, they may increase sedation or respiratory suppression.
Additionally, chronic opioid use can dampen ketamine’s analgesic effects. Doctors often adjust or temporarily suspend opioid regimens before therapy begins.Monoamine oxidase inhibitors (MAOIs), a class of older antidepressants, also present risk because they amplify ketamine’s effect on catecholamines, potentially leading to dangerous spikes in blood pressure.
The same applies to stimulants such as amphetamines or methylphenidate (used for ADHD), which can overactivate the cardiovascular system when combined with ketamine.Even supplements or over-the-counter products like St. John’s Wort may alter ketamine metabolism, increasing side effects like dizziness or nausea.
A comprehensive medication review is therefore one of the most critical steps before approval. By identifying risky overlaps early, clinicians can modify doses, pause certain prescriptions, or suggest safer timing between medications and infusions.
4. Lifestyle and Behavioral Factors That Can Affect Eligibility
Beyond diagnoses and prescriptions, lifestyle choices and behavior patterns can also determine candidacy. Even healthy individuals can be temporarily disqualified from ketamine therapy if certain habits or circumstances increase risk.
Frequent alcohol consumption or recreational drug use is one example. Because ketamine already influences perception and consciousness, adding alcohol or other psychoactive substances before or after sessions can create unpredictable reactions. Clinics generally require a period of sobriety before starting treatment.
Sleep deprivation, poor nutrition, and dehydration may sound minor, but they can affect how the body responds to ketamine. A dehydrated patient may experience stronger blood pressure fluctuations, while a malnourished one may metabolize the medication too slowly, leading to prolonged dissociation or nausea.


Driving or operating machinery immediately after sessions is also discouraged. People whose work or caregiving responsibilities prevent rest after each appointment may be temporarily disqualified until they can arrange adequate downtime. Successful ketamine therapy depends not only on what happens in the clinic but also on how patients care for themselves before and after each session.
Emotional readiness is another aspect. Some clinics evaluate a patient’s support system and coping capacity. Those undergoing major life crises like recent bereavement or unstable housing might be advised to postpone therapy. Ketamine can surface intense emotions, and without support, the experience can become overwhelming instead of healing.
5. Screening, Evaluation, and Responsible Use
The process of qualifying for ketamine therapy is as important as the treatment itself. Clinics that follow best practices start with a multi-step screening process involving medical questionnaires, psychiatric interviews, and sometimes lab work. This ensures that only individuals who can safely tolerate the treatment are approved.


A thorough evaluation doesn’t exist to exclude people, it exists to protect them.
Typically, the screening begins with a review of the patient’s physical health, including cardiovascular and respiratory function. Next comes a mental health history that explores trauma, substance use, and current emotional stability. Blood tests may check for underlying metabolic or hormonal conditions.

If everything looks favorable, a test dose or short observation session may follow before full treatment begins. During infusions, clinicians monitor heart rate, oxygen saturation, and blood pressure continuously. Some programs also include integration therapy, where patients discuss their experiences afterward to make sense of insights or emotions that surface during the session.
When clinics rush or skip these steps, risks multiply. But when done right, screening becomes a foundation for safe and lasting transformation. Ketamine therapy works best when both physical safety and emotional preparation align.
6. Comparing Eligible vs. Ineligible Candidates
To illustrate how screening shapes outcomes, here’s a simple comparison of two profiles often seen in clinics:
| Category | Eligible Candidate | Ineligible Candidate |
| Physical Health | Stable blood pressure and heart function; no respiratory issues | Uncontrolled hypertension or heart failure |
| Mental Health | Depression or PTSD without psychosis or mania | Active psychosis, untreated bipolar disorder |
| Medication Use | Non-conflicting antidepressants; no benzodiazepine overuse | High-dose benzos, opioids, or MAOIs |
| Lifestyle | Sober, well-rested, supportive environment | Ongoing substance use or unstable living conditions |
| Support System | Regular therapy or integration sessions | No follow-up care or mental health support |
| Motivation | Seeking healing and growth | Seeking dissociation or recreational use |
This table highlights how interconnected physical, mental, and social health are when deciding who qualifies. Safety depends not only on biology but also on mindset and readiness for meaningful change.
7. Myths About Ketamine Disqualification
Even as awareness grows, misconceptions persist about who can or cannot undergo ketamine therapy. Many people wrongly assume that a single diagnosis automatically disqualifies them when, in reality, it depends on control, stability, and monitoring.
For example, someone with high blood pressure may still qualify if their condition is well managed with medication. Similarly, patients with a past substance use disorder might be approved after sustained recovery and accountability measures are in place.
Another myth is that age itself is a disqualifier. While older adults may have more health risks, they can still benefit if evaluations show stable organ function. What matters is individualized assessment, not blanket exclusions.
Some also believe that ketamine therapy is reserved only for those in deep crisis. In truth, many patients begin treatment before their symptoms reach that stage, using it as an early intervention tool. Disqualification is rarely permanent; it’s more often a signal that additional preparation or stabilization is needed before proceeding.
By clearing up these myths, patients can approach the process with realistic expectations and focus on building readiness instead of fear.
How Ketamine Therapy Is Changing Trauma Recovery
Despite the eligibility limits, ketamine therapy is redefining the way trauma and emotional pain are treated. Unlike traditional antidepressants that take weeks to act, ketamine works within hours by increasing neuroplasticity and the brain’s ability to form new connections. This rapid rewiring allows people to confront traumatic memories with greater emotional distance and resilience, helping them process rather than relive their pain.
For veterans with PTSD, survivors of abuse, and first responders carrying invisible wounds, ketamine offers a bridge back to normal life. It’s often used alongside therapy sessions, where patients explore memories that once felt unbearable but now seem manageable.
The emotional clarity that follows ketamine sessions often inspires lifestyle changes better sleep, healthier eating, and renewed social engagement. Though not suitable for everyone, the therapy’s growing success stories continue to reshape mental health care.
As research deepens and screening protocols improve, more people will find themselves safely eligible for this life-changing approach.Ketamine therapy may not be for everyone, but for those who qualify, it represents a turning point one where science and compassion meet to heal trauma from the inside out.
