Ketamine infusions have gained recognition as an effective treatment for conditions such as depression, anxiety, and chronic pain, offering rapid relief when traditional medications fall short. The treatment’s growing popularity has brought new questions about safety and post-procedure recovery, especially regarding the ability to drive afterward.
Although the effects of ketamine fade within hours, its influence on reaction time, coordination, and cognition can persist beyond what patients initially perceive. Knowing when it is safe to resume driving helps protect not only the individual’s well-being but also public safety on the road.
How soon can you drive after Ketamine Infusion? Because each patient’s response to ketamine varies based on dosage, metabolism, and prior health conditions, medical professionals emphasize personalized guidance over fixed timelines.
Why Driving After Ketamine Infusion Requires Caution
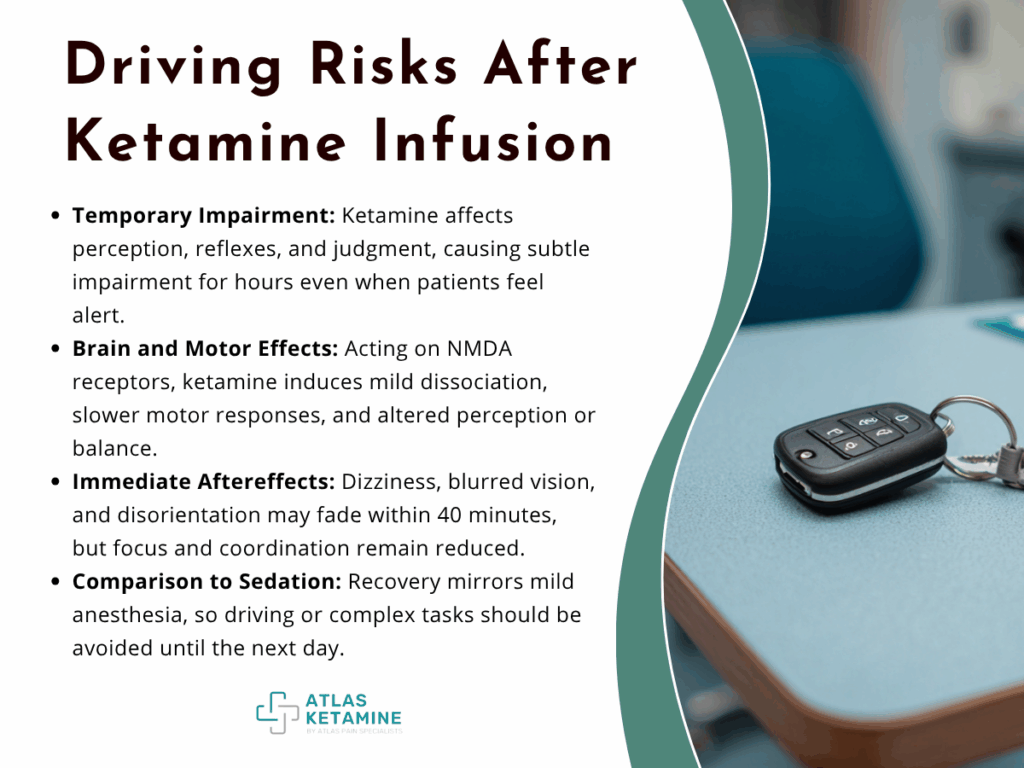
Ketamine alters neural activity in ways that temporarily affect perception, reflexes, and judgment. Even when patients feel alert shortly after treatment, subtle impairment may linger for several hours.
Medical experts universally recommend arranging transportation home after each session to prevent accidents or legal issues. Sedatives such as ketamine can influence psychomotor function beyond visible signs of drowsiness.
- How Ketamine Affects Coordination and Cognition
Ketamine acts on the brain’s NMDA receptors, interrupting certain neurotransmission pathways associated with pain and mood regulation. This same mechanism produces mild dissociation and delayed motor control, making precise movements more difficult.
Patients may underestimate these effects because cognitive clarity often returns before full physical coordination does. Studies have shown that even small doses can reduce reaction speed for several hours following administration.
Visual depth perception, balance, and time awareness can also shift temporarily, posing danger when operating a vehicle.
- Immediate Sedative Aftereffects
Right after infusion, most clinics monitor patients in recovery areas for twenty to forty minutes. During this time, mild dizziness, blurred vision, or disorientation are common but generally short-lived.
Even once these sensations subside, concentration lapses can persist. Driving under these conditions significantly increases the likelihood of collisions, particularly in heavy traffic or complex intersections.
Since ketamine is among the substances that impair the ability to safely operate a vehicle, refrain from driving until fully recovered.
- Comparison to Other Medical Sedations
The recovery pattern from ketamine resembles that of outpatient anesthesia used in dental or minor surgical procedures. Patients typically wait a full day before resuming driving or work activities requiring sustained focus.
Although ketamine is administered at lower doses in therapeutic settings, the cognitive effects remain similar in duration. Physicians therefore adopt the same post-care precautions as they would for mild anesthesia recovery.
Typical Recovery Timeline After Infusion
The length of recovery before driving depends on dosage, infusion rate, and the individual’s metabolism. Most patients require several hours before mental sharpness and motor control return completely.
Clinics in the American Association of Ketamine Physicians, Psychotherapists & Practitioners recommend avoiding driving for the remainder of the treatment day, allowing overnight rest before resuming normal activities.
- First Two Hours Post-Infusion
Immediately following the procedure, blood pressure and heart rate often fluctuate slightly due to the medication’s stimulant properties. Patients may feel light-headed or disconnected as neural pathways reestablish normal signaling.
During this period, supervision is essential, and clinics will not release patients to drive or take public transport alone. Many facilities require a companion to sign out the patient and confirm transportation arrangements.
- Four to Six Hours After Treatment
As plasma concentration declines, most individuals report gradual return of clarity and balance. However, coordination and short-term memory may still lag behind normal function.
Even if you feel fine, residual impairment can affect quick decision-making and emergency response on the road. For that reason, most providers continue to discourage driving until at least the next morning.
Hydration, nutrition, and rest can speed recovery by stabilizing blood pressure and supporting metabolism of the medication.
- The Following Morning
After eight to twelve hours of rest, most patients can safely resume daily routines, including driving. Clinicians advise a self-assessment for fatigue or lingering confusion before returning to traffic.
Patients receiving high-dose or multi-day infusions may experience cumulative sedation and should discuss timelines with their care team. Documenting your response to early sessions helps determine your personal safe window for driving in future treatments.
Factors That Influence Driving Readiness

Recovery time after ketamine treatment is not universal, as individual physiology and environmental conditions contribute to differences in response. Medical history, concurrent medications, and dosage schedule each play measurable roles in determining recovery speed and clarity.
- Dosage and Administration Method
Higher infusion doses extend dissociative effects and delay full motor recovery. Clinics adjust dosage based on therapeutic goals, often varying between pain management and psychiatric protocols.
Continuous low-dose infusions for chronic pain may produce less immediate sedation but still alter reaction time for several hours. Intramuscular or intranasal administrations can also yield longer residual effects depending on absorption rate.
- Metabolic and Health Differences
Age, liver function, and overall cardiovascular health significantly affect ketamine metabolism. Patients with slower metabolic rates may require longer observation before leaving the clinic.
Dehydration or lack of sleep before treatment can amplify post-infusion fatigue. Following pre-procedure instructions on rest and hydration supports faster recovery and safer post-treatment mobility.
- Medication Interactions
Ketamine’s interaction with other central nervous system depressants, including benzodiazepines, opioids, or alcohol, intensifies sedation. Patients taking antidepressants or antihistamines may also experience prolonged reaction time.
Before each infusion, disclose all current prescriptions and supplements to your provider. Adjusting scheduling or dosage prevents dangerous overlap of sedative effects after treatment.
Post-Infusion Guidelines for Safe Transportation
Adhering to post-treatment transportation protocols ensures patient safety and compliance with medical best practices. Clinics emphasize planning ahead rather than improvising transportation after infusion.
Having a designated driver or pre-booked ride service eliminates risk during the vulnerable recovery window.
- Clinic Discharge Policies
Most ketamine clinics refuse to release patients who arrive without a driver or arranged transport. Responsible discharge policies are integral to patient safety and regulatory compliance.
Before your appointment, confirm the clinic’s release criteria, as some require the driver to remain on-site throughout the session. Compliance prevents rescheduling and reinforces the clinic’s duty of care.
- Alternative Transportation Options
If no companion is available, plan for rideshare or taxi services before arriving at the clinic. Scheduling a pickup window prevents confusion during post-infusion grogginess.
Some medical centers partner with local transportation programs for patients undergoing outpatient therapy. Ask about available arrangements during consultation to avoid last-minute delays.
- Communicating With Employers or Family
Because treatment sessions may occur multiple times weekly, inform employers or family about the temporary driving restrictions. Arranging flexible schedules reduces stress and promotes adherence to medical advice.
Employers familiar with therapeutic infusion therapy often accommodate modified work hours following treatment days. Transparent communication reinforces safety and prevents misunderstandings about recovery time.
Legal and Ethical Considerations
Operating a vehicle after sedation raises not only safety issues but also legal liability. Driving while under the lingering influence of ketamine may be considered impaired operation under state law.
Patients must treat post-infusion impairment with the same caution applied to alcohol or controlled substances.
- Impaired Driving Regulations
State laws prohibit driving under any condition that compromises cognitive or physical control. If an accident occurs, presence of ketamine, even if prescribed, can result in legal scrutiny.
Patients should retain treatment documentation and discharge times to verify compliance with medical recommendations. Keeping written confirmation of transportation plans adds another layer of protection.
- Employer and Insurance Policies
Some employers require disclosure of sedative treatments when work involves driving or heavy machinery. Failing to report temporary impairment could jeopardize occupational safety compliance.
Auto insurance claims following an accident may face denial if evidence suggests post-medical sedation. Observing a conservative no-drive period shields both reputation and coverage eligibility.
- Informed Consent and Patient Responsibility
Every clinic’s consent form outlines the expectation that patients refrain from driving for at least twenty-four hours. Signing that document creates a binding acknowledgment of understanding.
Following these terms is not only ethical but also a sign of respect for medical protocol and public safety. Adherence reinforces trust between patient and practitioner, ensuring continued access to care.
How to Prepare for a Smooth Recovery
Preparation before and after infusion directly affects how quickly normal function returns. Simple planning eliminates stress and supports full recovery within the safest timeframe.
Consistent routines across sessions make it easier to anticipate your body’s response and manage transportation logistics efficiently.
- Pre-Infusion Steps
Eat a light meal a few hours before treatment and avoid caffeine or alcohol the night before. Arriving well-rested enhances tolerance and stabilizes blood pressure during the session.
Confirm that your driver or ride service knows the estimated completion time. Keeping emergency contact information on file ensures seamless coordination with clinic staff.
- Aftercare and Monitoring
Once home, rest in a calm environment away from bright light or loud noise. Drink water regularly to aid elimination of the medication from your system.
Avoid operating any machinery, signing documents, or making major decisions until the following day. Mental rest complements the therapeutic effects and allows your body to integrate the benefits of the infusion.
- Building a Routine for Ongoing Treatments
If undergoing a series of infusions, track how you feel after each session. Noting fatigue levels, mood changes, and cognitive clarity helps tailor future schedules.
Some patients find morning sessions more convenient, allowing full recovery before the next day. Coordinating rides and post-infusion rest around a consistent timeline improves safety and comfort across the treatment plan.
What to Do After a Ketamine Infusion: Post-Treatment Care
Recovery after a ketamine infusion extends beyond the clinic visit, requiring deliberate rest and attention to subtle physical and emotional changes. Allowing the body to stabilize before resuming daily tasks ensures that the therapy delivers its full benefit without unnecessary strain.
Most patients find that quiet rest, hydration, and balanced nutrition accelerate recovery and minimize post-infusion fatigue. Avoiding screens and bright lights for several hours helps the nervous system recalibrate while supporting mental clarity the next day.
Communicating any side effects or mood changes with your care team maintains treatment safety and effectiveness over time. Tracking responses between sessions also helps clinicians fine-tune dosage and scheduling for optimal outcomes.
