Depression is a serious problem in today's world, impacting millions of people due to its widespread influence on mental well-being. A strange paradox does, however, surface amid the complexity of this condition: ketamine, a drug frequently linked to eliciting depressed symptoms, may also be a promising treatment for depression.
Depression's impact extends far beyond mere feelings of sadness, encompassing a spectrum of symptoms that disrupt daily life and erode one's sense of well-being. Research suggests that chronic Ketamine use can indeed lead to depressive episodes, with users reporting feelings of despair, lethargy, and emotional numbness. Let as begin addressing depression with ketamine.
Depression and Ketamine
Depression is a complex mental illness that is characterized by enduring sadness and negative emotions as well as a lack of interest in or enjoyment from once-enjoyed activities. Beyond these core symptoms, depression can manifest in various ways, including changes in appetite and sleep patterns, difficulty concentrating, fatigue, and even thoughts of self-harm or suicide.
Ketamine's association with depression may seem paradoxical at first glance. Traditionally known as a dissociative anesthetic used in medical settings, Ketamine has also gained notoriety as a recreational drug, often associated with altered states of consciousness and depressive symptoms.

Ketamine's Association with Depressive Symptoms
While Ketamine's primary use as an anesthetic is well-established, its effects on mood regulation have garnered increasing attention in psychiatric research. Studies have shown that chronic Ketamine use can lead to a phenomenon known as "Ketamine-induced depression," characterized by persistent feelings of sadness, dysphoria, and anhedonia.
The phenomena's complicated and varied causes include modifications to neurotransmitter systems, specifically glutamate, and adjustments to neuroplasticity in the brain's dopamine network.
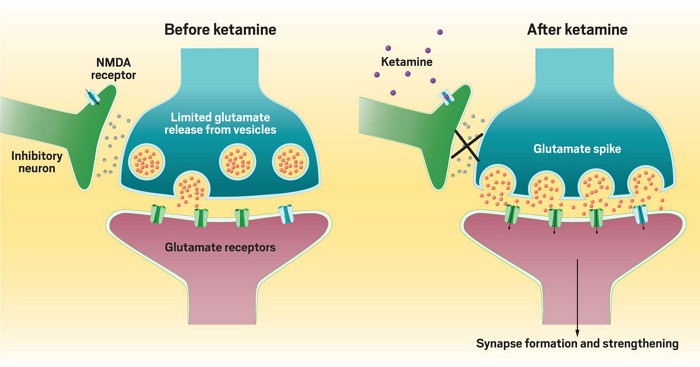
- One proposed mechanism is the dysregulation of glutamatergic neurotransmission, leading to disruptions in synaptic plasticity and neural circuitry implicated in mood regulation. Ketamine's acute effects on glutamate release and receptor function may contribute to initial feelings of euphoria or dissociation, followed by rebound dysphoria as the drug's effects wear off.
- Additionally, Ketamine's impact on other neurotransmitter systems, such as dopamine and serotonin, further complicates its relationship with depression. While acute Ketamine use may induce transient improvements in mood, chronic exposure can lead to neuroadaptive changes that contribute to the development of depressive symptoms over time.
The Paradoxical Potential of Ketamine in Depression Treatment
Despite its association with depressive symptoms, Ketamine also holds promise as a novel and rapidly acting treatment for depression. This apparent paradox has sparked considerable interest among researchers and clinicians seeking new approaches to managing treatment-resistant depression.
Unlike traditional antidepressants, which may take weeks to months to exert their therapeutic effects, Ketamine has been shown to induce rapid and robust antidepressant effects within hours of administration. On the other hand, chronic Ketamine use has been linked to the development of depressive symptoms, with individuals experiencing dysphoria, anhedonia, and other mood disturbances following prolonged exposure.
Mechanisms Underlying Ketamine-Induced Depression
Ketamine's acute effects on glutamate release and N-methyl-D-aspartate (NMDA) receptor function may initially induce feelings of euphoria or dissociation, but chronic exposure can lead to neuroadaptive changes that contribute to the development of depressive symptoms. Dysregulation of synaptic plasticity within key brain regions implicated in depression, such as the prefrontal cortex and hippocampus, may further worsen mood disturbances and contribute to the progression of Ketamine-induced depression over time.
In addition, Ketamine's effects on other neurotransmitter systems, including dopamine and serotonin, may also play a role in the development of depressive symptoms. Dysregulation of these neurotransmitter systems can disrupt the delicate balance of mood regulation, leading to the emergence of depressive symptoms in vulnerable patients.
The Antidepressant Potential of Ketamine
Despite its association with depressive symptoms, Ketamine also possesses remarkable antidepressant properties that have captured the interest of researchers and clinicians alike. The discovery of Ketamine's rapid and strong antidepressant effects has revolutionized the field of psychiatry, offering new hope for individuals suffering from treatment-resistant depression.
Ketamine may offer a unique mechanism for alleviating depressive symptoms by promoting the growth of new synaptic connections and restoring synaptic function. Moreover, Ketamine's rapid onset of action makes it particularly well-suited for individuals experiencing acute suicidal ideation or severe depressive episodes where immediate relief is paramount.
The efficacy of Ketamine therapy in treating depression has been demonstrated in numerous clinical trials and research studies. Meta-analyses have consistently shown that Ketamine produces significant improvements in depressive symptoms, with response rates ranging from 50% to 70% among treatment-resistant patients.
Moreover, Ketamine has been found to be effective across various subtypes of depression, including major depressive disorder, bipolar depression, and post-traumatic stress disorder (PTSD), highlighting its broad applicability as a treatment option.
Mechanisms Underlying Ketamine's Antidepressant Effects
The antidepressant effects of Ketamine are thought to come from its unique mechanism of action, which differs from that of traditional antidepressant medications. While traditional antidepressants primarily target monoaminergic neurotransmitter systems, such as serotonin, norepinephrine, and dopamine, Ketamine acts on the glutamatergic system, specifically targeting the N-methyl-D-aspartate (NMDA) receptor.
Ketamine's blockade of the NMDA receptor leads to downstream effects that promote synaptic plasticity and the formation of new neural connections in key brain regions implicated in depression, such as the prefrontal cortex and hippocampus. These neuroplastic changes are believed to underlie the rapid and sustained antidepressant effects observed with Ketamine therapy.
Additionally, Ketamine's modulation of other neurotransmitter systems, including gamma-aminobutyric acid (GABA), opioid, and cannabinoid receptors, may also contribute to its antidepressant properties.
Balancing The Risks and Benefits Of Ketamine Therapy
Ketamine therapy is typically administered via intravenous infusion or intranasal spray in a controlled clinical setting under the supervision of trained medical professionals. The dosing and frequency of Ketamine treatments may vary depending on individual patient factors, such as the severity of depression, treatment response, and tolerability.
Long-term maintenance of Ketamine therapy may involve periodic booster infusions or transition to alternative maintenance treatments, such as oral Ketamine or other adjunctive therapies.

1. The Ethical Considerations
As with any medical intervention, the use of Ketamine therapy for depression necessitates careful consideration of ethical principles and patient well-being. While Ketamine has demonstrated rapid and robust antidepressant effects, ethical concerns arise regarding its potential for misuse, abuse, and diversion.
Given Ketamine's history as a recreational drug and its classification as a controlled substance, clinicians must exercise caution in prescribing and monitoring Ketamine therapy to minimize the risk of misuse and diversion. Moreover, the high cost of Ketamine therapy may pose accessibility barriers for some individuals, raising questions about equity and social justice in mental health care.
As Ketamine therapy becomes more widely adopted, efforts must be made to ensure equitable access to treatment for all individuals, regardless of socioeconomic status or insurance coverage. Additionally, ongoing research is needed to evaluate the long-term safety and efficacy of Ketamine therapy and to identify strategies for optimizing treatment outcomes while minimizing potential risks.
2. Potential Risks and Adverse Effects
While Ketamine therapy is generally well-tolerated, it is not without risks, and careful consideration must be given to potential adverse effects. Transient side effects, such as dissociation, dizziness, nausea, and increased blood pressure, are commonly reported during and immediately following Ketamine infusion.
These side effects are typically mild to moderate in severity and resolve spontaneously within hours of treatment. However, more serious adverse effects, such as hallucinations, psychosis, and cardiovascular complications, may occur, particularly at higher doses or in individuals with pre-existing medical conditions.
Close monitoring of patients during and after Ketamine therapy is essential to identify and manage any adverse effects that may arise promptly. Additionally, comprehensive psychiatric evaluation and screening are crucial to identify individuals at higher risk for adverse reactions and to tailor treatment approaches accordingly.
Clinical Applications and Considerations
Ketamine therapy is usually administered in a controlled clinical setting under the supervision of qualified and trained medical professionals. The route of administration may vary depending on patient factors and treatment goals, with intravenous infusion and intranasal spray being the most common methods.
The dose and frequency of Ketamine treatments are tailored to each individual based on factors such as the severity of depression, treatment response, and tolerability. During Ketamine infusion, patients are closely monitored for vital signs, adverse reactions, and changes in mental status.
Clinicians may use standardized rating scales, such as the Montgomery-Åsberg Depression Rating Scale (MADRS) or the Quick Inventory of Depressive Symptomatology (QIDS), to assess treatment response and track symptom improvement over time. Monitoring and evaluation are important to ensure patient safety, optimize treatment outcomes, and adjust treatment plans.
1. Integration with Adjunctive Therapies
Ketamine therapy is often integrated into a comprehensive treatment plan that may include adjunctive therapies to address the multifaceted nature of depression. Psychotherapy, like cognitive-behavioral therapy (CBT) or mindfulness-based therapies, can help patients develop coping skills, challenge negative thought patterns, and cultivate resilience.
Psychosocial support, peer support groups, and community resources can also provide valuable support and encouragement throughout the treatment process. In addition to psychotherapy, lifestyle modifications, such as regular exercise, healthy nutrition, adequate sleep, and stress management techniques, are important in promoting overall well-being and enhancing treatment outcomes.
2. Long-Term Treatment Considerations
While Ketamine therapy has demonstrated rapid and robust antidepressant effects, questions remain regarding the optimal duration and frequency of treatment, as well as the long-term maintenance of treatment response. Some individuals may experience sustained improvements in depressive symptoms following a course of Ketamine therapy, while others may require periodic booster infusions or transition to alternative maintenance treatments.
Long-term monitoring and follow-up care are essential to assess treatment response, monitor for relapse or recurrence of depressive symptoms, and identify any emerging concerns or adverse effects. Clinicians should collaborate closely with patients to develop individual treatment plans that address their unique needs, preferences, and goals.
3. Advancements in Ketamine Therapy
The future of Ketamine therapy holds promise for further advancements in treatment approaches, optimization of protocols, and refinement of delivery methods. Ongoing research efforts seek to elucidate the underlying mechanisms of Ketamine's antidepressant effects, paving the way for the development of novel pharmacological agents that target specific molecular pathways implicated in depression.
Additionally, innovative delivery systems, such as sustained-release formulations or intranasal devices, may offer improved convenience, safety, and tolerability for patients undergoing Ketamine therapy. Emerging evidence suggests that Ketamine therapy may have applications beyond depression, including the treatment of other psychiatric disorders such as anxiety disorders, obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD).
Ketamine Treatment For Bipolar Depression
The relationship between Ketamine treatment for bipolar depression shares similarities with the broader topic of depression while also presenting distinct considerations. Mechanistically, Ketamine's modulation of glutamatergic neurotransmission and promotion of synaptic plasticity underlie its rapid antidepressant effects, observed in both unipolar and bipolar depression.
Nonetheless, diagnosing and treating bipolar depression entails unique challenges due to the alternating episodes of depression and mania or hypomania characteristic of the disorder. Integrating Ketamine therapy into a comprehensive treatment plan requires careful consideration of these adjunctive treatments and their potential interactions.
Long-term management of bipolar depression involves maintaining mood stability and preventing the recurrence of depressive and manic/hypomanic episodes. Patient education about the risks and benefits of Ketamine therapy, medication adherence, and regular monitoring is crucial for optimizing treatment outcomes and promoting self-management in individuals with bipolar depression.
