If you’re here, chances are you’ve been wondering how something like ketamine could have anything to do with healing from deep psychological pain. Maybe you've heard people mention it in the context of therapy, or maybe you're exploring new treatment options far from the traditional ones.
Dissociative Identity Disorder (DID) is often misunderstood, even in spaces that claim to be mental health aware. If you live with it, or love someone who does, you already know it’s about surviving what felt unsurvivable, in a way the brain figured out on its own.
You live with trauma and in a system shaped by it. That’s not easy, and traditional therapies don’t always speak to every layer of that experience. So how does ketamine fit into this?
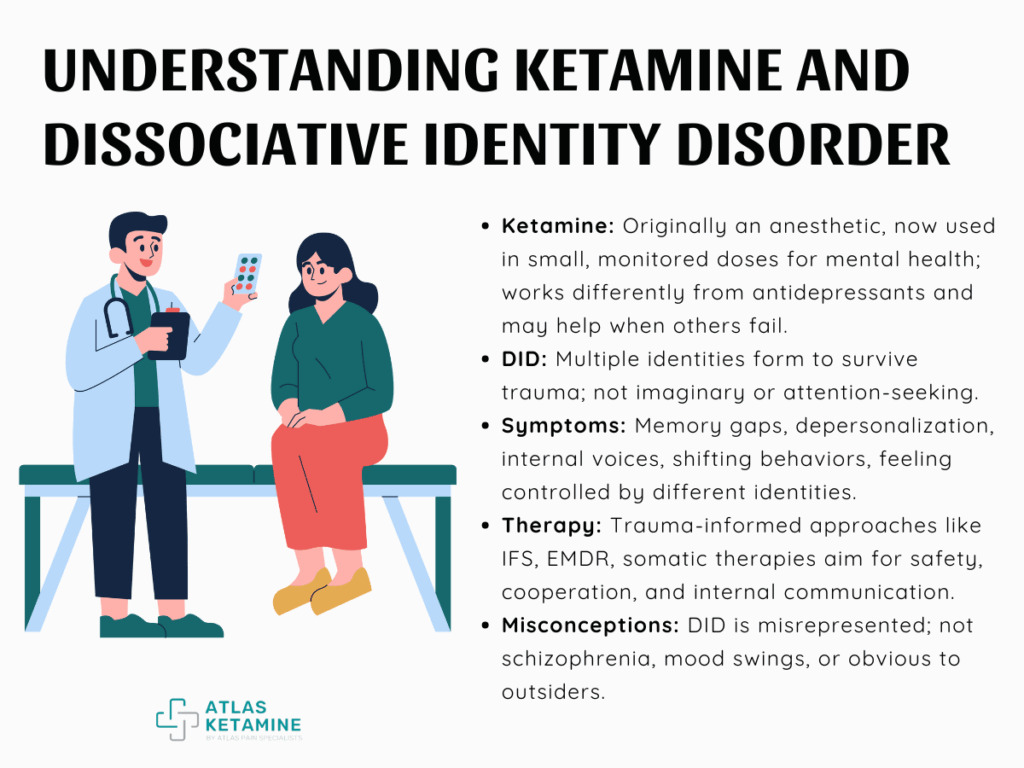
What Ketamine Really Is
New treatments or mental health terms can be overwhelming, especially when they touch on personal experiences that already carry a lot of weight. Before moving into the deeper questions, it helps to get familiar with what each part of this conversation actually means.
You might have heard about ketamine in passing or seen DID mentioned in ways that didn’t feel accurate. Ketamine is not new, but its role in mental health has shifted.
- It started out in medical settings as an anesthetic and later showed up in less controlled spaces, which gave it a reputation that many still associate with risk or misuse. That past can make it harder to see its potential role in healing.
- In more recent years, researchers and therapists began noticing that ketamine, in small monitored doses, may help ease certain mental health symptoms. It doesn’t work the way typical antidepressants do, and it doesn’t need to be taken daily.
That makes it stand out, especially for people who feel stuck in patterns that haven’t responded to other medications.
Dissociative Identity Disorder
When people talk about DID, it’s often through the lens of media or outdated ideas. That kind of portrayal rarely reflects what it actually feels like to live in a system.
It can leave you unseen, misrepresented, or even dismissed, which makes seeking support harder than it should be. DID forms as a way to survive early trauma that felt unbearable at the time.
The mind finds ways to separate experiences, memories, and emotions so that life can continue. These separate parts or identities often carry their own thoughts, needs, and roles. It’s not imaginary, it’s not attention-seeking, and it’s definitely not rare.
| Dissociative Identity Disorder (DID) | Description |
|---|---|
| Definition | A complex psychological condition where a person has two or more distinct identity states (also called "parts" or "alters") that may control behavior at different times. It forms as a response to severe trauma, usually in early childhood. |
| Cause | Typically linked to repeated childhood trauma, such as abuse or neglect. The brain creates separate identity states to survive overwhelming experiences. |
| Symptoms | Memory gaps (dissociative amnesia), feeling disconnected from self or surroundings (derealization/depersonalization), hearing internal voices, changes in handwriting or preferences, and feeling like “someone else” is in control. |
| Common Myths | DID is not the same as schizophrenia, it is not about “crazy mood swings,” and it’s not always obvious. It’s often portrayed inaccurately in media. |
| System | A term used to describe the whole group of parts/identities in one person. Each part often has specific roles (e.g., protector, caretaker, holder of trauma). |
| Diagnosis | Made by a licensed mental health professional through interviews and assessment tools. It requires ruling out other conditions. |
| Therapy Options | Trauma-informed therapy, Internal Family Systems (IFS), EMDR (if appropriate), and somatic approaches. The goal is safety, communication, and cooperation between parts—not necessarily fusion. |
What Makes DID So Complex?
Living with Dissociative Identity Disorder often means carrying layers of experience that don’t fit neatly into a single narrative. It’s not something that can be summed up in a few traits or explained by a short definition.
What makes DID hard to understand from the outside is exactly what makes it so real on the inside. You might already know how tiring it can be to explain yourself to people who think DID is just “switching personalities” or confusion.
DID Is Not Just About “Multiple Personalities”
Movies and media often reduce DID to sudden, dramatic changes in behavior. That makes it easy for people to miss the more common experiences, like losing time, feeling disconnected from your body, or hearing internal dialogue between parts.
These parts aren’t made up or random but exist for a reason. Each part usually has a role.
Some carry memories, some protect the system, some handle daily tasks. They don’t always get along, and they don’t always agree on what’s safe. But they all share one body, and over time, they form a system that learns how to function.
How Trauma Shapes the Mind
Early trauma can rewire how your brain stores information, reacts to stress, and even develops identity. When overwhelming things happen repeatedly and safety is never guaranteed, the mind starts to organize experience in a way that spreads the impact.
Instead of one steady sense of self, DID systems often build separate containers for different kinds of pain, memory, or emotion. You may not remember everything, but parts of you do.
You may not feel the fear right away, but someone inside holds it. This layered experience can be exhausting, but it also shows how powerful the human mind can be when it’s trying to survive.
Living with DID Day to Day
There’s no single way DID looks from the outside. Some people manage jobs, relationships, and responsibilities while switching between parts without anyone noticing.
Others might feel more fragmented, struggling with memory gaps or changes in behavior that feel out of their control. Both experiences are valid.
Daily life might involve internal conversations, negotiation, or conflict. It might mean losing time, finding things moved, or waking up in a place you don’t remember going.
Where Ketamine Comes In
Ketamine and DID may not seem like they belong in the same conversation. One is a drug often linked to anesthesia or depression treatment, the other a complex trauma response shaped over time.
But when traditional therapies aren’t reaching certain places, people start looking at different tools. Not out of desperation, but from a quiet, honest need for something that might finally meet them where they are.
Why Some People with DID Are Exploring Ketamine
Standard therapy can feel limited when trauma responses live deep in the body and mind. You might show up, sit on the couch, and try to talk but parts of you may not feel safe enough to share, or even stay present.
Ketamine has the potential to soften those walls, at least temporarily, so that therapy doesn’t feel like such a fight. Emotions or memories that normally feel too dangerous to approach become more reachable.
It doesn’t guarantee breakthroughs, but it sometimes helps a part of the system feel heard in ways that never felt possible before. That alone can shift things.
What Therapy Looks Like When Ketamine Is Involved
Therapy that includes ketamine is often done with a trained professional, sometimes with a therapist present during the experience. It may be done with sessions scheduled before and after to help you process what came up.
During a session, you might feel detached, emotional, calm, or even disoriented. That’s why having someone nearby who understands trauma and dissociation makes all the difference.
After the effects wear off, integration becomes the focus.
Potential Benefits for Trauma and Dissociation
For people with DID, dissociation is not a side effect but a language. Ketamine interacts with that language in a way that can either help or complicate things, depending on the timing, environment, and support in place.
In the right setting, it may help your system connect, communicate, or find some relief from long-held tension. These moments aren’t guaranteed, but when they happen, they can offer something that feels both new and deeply familiar.
What We Know and What We Don’t
When something feels new or unfamiliar, it’s easy to hope for clear answers. With ketamine and DID, though, the truth sits somewhere in the middle.
There’s growing curiosity and early research, but there’s also a lot we still don’t fully understand. And when it comes to something as personal as your mind, that uncertainty matters.
The Research So Far Is Still Early
Most of what we know about ketamine in mental health comes from studies on depression and PTSD. These studies show that ketamine can reduce certain symptoms, sometimes within hours, especially when nothing else has helped.
That’s part of what made people start looking at its potential beyond just mood disorders. But DID hasn’t been studied in the same way.
There are almost no large-scale studies focused specifically on how ketamine affects people with dissociative disorders. What that means is, the research isn’t saying “this doesn’t work”—it’s saying “we don’t fully know yet.”
Risks and Concerns
Like any treatment, ketamine isn’t risk-free. It can amplify certain thoughts or feelings, and for someone who already experiences dissociation regularly, it might stir things up in ways that are hard to manage without the right structure.
There’s also the issue of access. Not all providers understand DID, and not all ketamine clinics are built with trauma-informed care in mind.
That gap can make things harder.
Things to Think About Before Trying Ketamine
This isn’t a choice to make lightly, and it shouldn’t be. Trying ketamine as part of your healing process can be deeply personal, and there’s no “right” feeling to have about it.
Curiosity, doubt, hope, fear all belong. You’re allowed to ask questions without pressure and take as much time as you need before moving forward.
The Right Therapist
A therapist who understands trauma, dissociation, and systems can help you explore whether ketamine fits into your healing or not. The key word here is understands, someone who won’t brush off your parts, rush the process, or push their own agenda.
The right therapist will listen not just to what you're saying but how your system responds. They’ll help you explore what safety would need to look like before, during, and after a session. You deserve that kind of care.
And if someone dismisses your concerns or treats this like a quick fix, that’s a sign to keep looking.
Setting, Support, and Safety
The setting you’re in while experiencing ketamine makes a huge difference. Do you feel emotionally safe with the person guiding the session? Do you have a plan for what happens afterward? These things are essential.
Some people choose to have a trusted therapist or support person present. Others make sure they have space afterward to rest, reflect, or reconnect with their parts.
Going into a session without a clear support structure can leave you feeling exposed, and that can undo more than it helps. Thoughtful planning can make the experience feel held, not chaotic.
What Informed Consent Should Actually Look Like
Informed consent is a conversation, one where you fully understand what the experience might be like, what risks come with it, and what steps will be taken to support you through it. You shouldn’t feel rushed, and you shouldn’t have to guess what’s going to happen.
This also means knowing what happens after. How will the experience be integrated into your ongoing therapy? What if something unexpected comes up?
You deserve to know exactly what you're walking into, and you have every right to say no, pause, or change your mind at any point in the process.
How Much Does a Ketamine Infusion Cost
Living with DID means navigating life in a way most people don’t see or understand. So when you think about what might help, it makes sense to look beyond traditional routes.
Part of that process involves more than just the emotional and therapeutic pieces. Cost is a real factor, and one that can impact whether this option is even accessible.
Ketamine infusions can be expensive, especially since they’re often not covered by insurance. That reality can be frustrating when you’re already carrying the weight of complex trauma and seeking care that actually works for you.
