Obsessive-Compulsive Disorder (OCD) is a debilitating mental health condition marked by intrusive thoughts and repetitive behaviors that can consume hours of a person’s day. While traditional treatments like selective serotonin reuptake inhibitors (SSRIs) and cognitive behavioral therapy (CBT) have helped many manage their symptoms, a significant portion of individuals often labeled “treatment-resistant” see little to no relief.
This has pushed researchers to explore alternative solutions, including ketamine, a drug originally used as an anesthetic.
Understanding OCD and Why Traditional Treatments Fall Short
Obsessive-Compulsive Disorder (OCD) is a chronic mental health condition marked by a cycle of intrusive thoughts (obsessions) and repetitive behaviors (compulsions). These patterns can be overwhelming, distressing, and time-consuming, interfering with daily functioning, relationships, and quality of life.
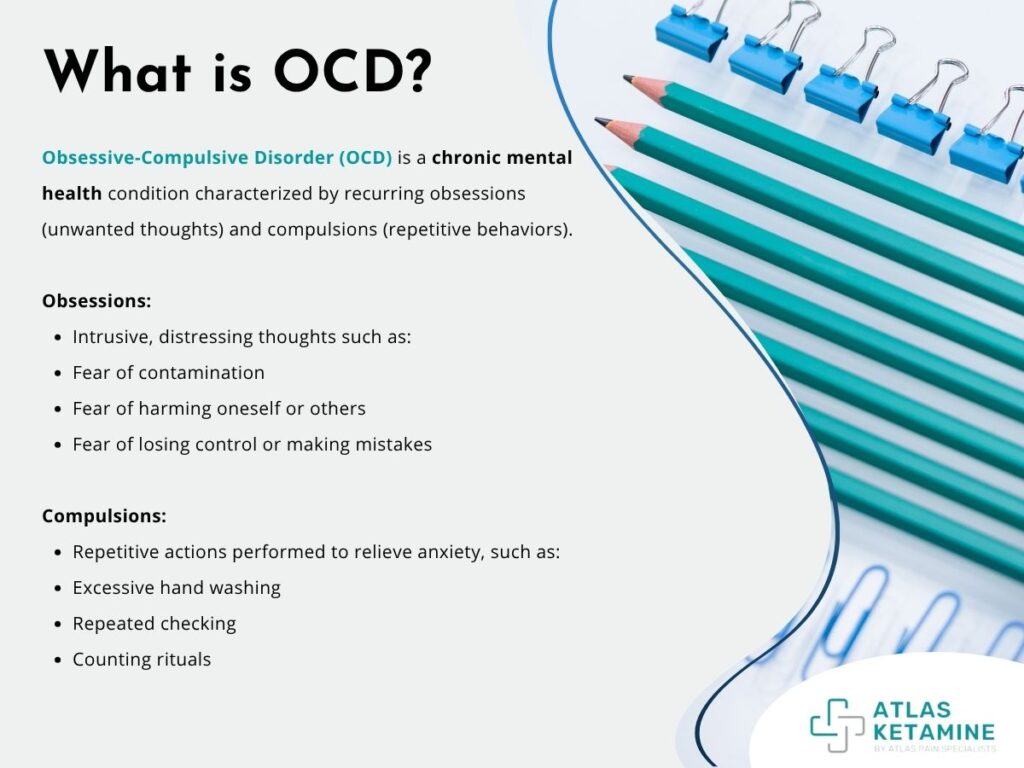
Common obsessions include fears of contamination, harm, or losing control, while compulsions might involve excessive hand washing, checking, or counting rituals meant to relieve anxiety.
Traditional treatments for OCD typically include selective serotonin reuptake inhibitors (SSRIs) and cognitive behavioral therapy (CBT), especially a form called exposure and response prevention (ERP). While these options have helped many people manage their symptoms, they are not universally effective.
SSRIs can take weeks or months to show results and may cause side effects like fatigue, weight gain, or emotional blunting. ERP requires time, commitment, and emotional stamina, which can be difficult for individuals with severe or complex symptoms.
Unfortunately, a significant portion of individuals with OCD, estimated at 30–40%, do not experience meaningful improvement with standard treatments. This treatment-resistant OCD has prompted researchers and clinicians to explore alternative therapies, including newer medications, neuromodulation techniques, and more recently, the use of ketamine as a potential fast-acting option.
What Is Ketamine and How Does It Work?
Ketamine is a well-known anesthetic that has been used in medical settings since the 1960s for pain relief and sedation during surgery. More recently, it has gained attention for its rapid-acting antidepressant effects, especially in patients who don’t respond to traditional treatments.
Unlike most antidepressants that target serotonin or dopamine, ketamine works primarily on the brain’s glutamate system. Below is how ketamine works:
Targeting the Glutamate System
Ketamine operates primarily through the brain's glutamate system, which is crucial for mood regulation, learning, and memory. Unlike traditional antidepressants that focus on serotonin or dopamine, ketamine's effects are driven by changes in glutamate signaling.
Blocking the NMDA Receptor
The key mechanism of ketamine is its ability to block the N-methyl-D-aspartate (NMDA) receptor, a critical component in glutamate transmission. This action alters the brain's normal communication pathways, contributing to its rapid effects.
Resetting Neural Pathways
By interfering with the NMDA receptor, ketamine helps "reset" certain overactive neural circuits that may contribute to conditions like OCD. This reset is thought to reduce the intensity of obsessive thoughts and compulsions.
Promoting Neuroplasticity
One of the critical effects of ketamine is its ability to promote neuroplasticity, the growth of new neural connections. This synaptic growth allows the brain to form new patterns of thinking and behavior, which can be essential in breaking the repetitive cycles of OCD.
Rapid Onset and Short-Term Relief
Due to its fast-acting nature, ketamine can provide rapid symptom relief, often within hours. While these effects may be temporary, the quick improvement in mood and cognitive flexibility is what makes ketamine particularly interesting for treating OCD.
The Risks and Side Effects of Ketamine Therapy for OCD
While ketamine shows promise for treating OCD, it is important to understand the potential risks and side effects that may accompany its use. Like any medical treatment, ketamine therapy is not without its challenges, and it is essential for individuals to weigh the benefits against the potential downsides.
Short-Term Side Effects
In the short term, ketamine can cause dissociation, where individuals may feel detached from their surroundings or their own body. This can be disorienting or uncomfortable but typically wears off as the drug’s effects subside.
Other common side effects include nausea, dizziness, and elevated blood pressure, particularly when administered in higher doses or during infusions. These side effects are generally temporary and resolve quickly after the treatment ends.
Long-Term Concerns
While short-term effects are usually manageable, the long-term safety of repeated ketamine use remains a concern. Ketamine has been associated with bladder issues in individuals who use it recreationally or in high doses over extended periods.
Additionally, there is the potential for psychological dependence in some individuals, particularly if used frequently without appropriate supervision or medical oversight.
Psychiatric Risks
Ketamine’s powerful effects on the brain's neurotransmitter systems mean it may not be suitable for people with certain psychiatric conditions, such as untreated psychosis or bipolar disorder. The drug may exacerbate symptoms or trigger new mental health challenges in vulnerable individuals.
Medical Supervision is Crucial
Given these risks, ketamine therapy for OCD must always be conducted in a controlled medical environment under the supervision of professionals trained in administering the drug. Patients should be carefully monitored throughout the process to manage any adverse effects and ensure safety.
Who Might Benefit from Ketamine Therapy for OCD?
Ketamine therapy offers hope for individuals with treatment-resistant OCD, especially those who have not found relief from traditional treatments like SSRIs or cognitive behavioral therapy (CBT).
For those struggling with severe symptoms, ketamine may provide rapid symptom relief, offering a temporary "mental reset" that helps break free from the cycle of obsessive thoughts and compulsive behaviors. In this section, we'll explore who is most likely to benefit from ketamine therapy and how it can be integrated into a broader treatment plan.
Individuals with Treatment-Resistant OCD
Ketamine therapy can be highly beneficial for individuals with treatment-resistant OCD, those who have not found relief from conventional treatments such as SSRIs, cognitive behavioral therapy (CBT), or exposure and response prevention (ERP). These individuals often continue to struggle with intrusive thoughts and compulsive behaviors despite trying multiple therapies, leaving them in search of alternative options.
Rapid Relief for Severe Symptoms
For those who have not responded to traditional treatments, ketamine offers the potential for rapid symptom reduction. Many patients report experiencing a temporary mental reset after receiving ketamine therapy, which helps them break free from persistent obsessive thoughts and compulsive actions. This immediate relief can be particularly valuable, allowing individuals to engage more effectively in therapy or daily activities and helping them achieve greater mental clarity during their treatment.
Enhanced Therapy Integration
Ketamine therapy can be particularly useful when combined with ongoing CBT or ERP. The temporary reduction in symptoms allows individuals to better engage in these therapeutic methods, reinforcing healthier thought patterns and behaviors that contribute to long-term improvement.
Key Candidate Traits
People who might benefit most from ketamine therapy typically have severe OCD that hasn’t responded to traditional methods, and they are open to trying an alternative, experimental approach. These individuals are looking for relief from the intensity of their symptoms and may be prepared for repeated treatments to maintain the benefits, as the effects of ketamine can often be short-lived.
Comparing Ketamine to Traditional OCD Treatments
When considering treatment options for OCD, it’s essential to compare ketamine with traditional therapies, such as selective serotonin reuptake inhibitors (SSRIs), cognitive behavioral therapy (CBT), and exposure and response prevention (ERP). While these conventional treatments have proven effective for many, they may not work for everyone, and ketamine offers a potential alternative for individuals with treatment-resistant OCD.
Speed of Action
One of the most significant differences between ketamine and traditional treatments is the speed of action. SSRIs and CBT, the primary treatments for OCD, often take weeks or even months to show significant results. This can be frustrating for individuals experiencing persistent, severe symptoms. In contrast, ketamine offers rapid relief, with some patients experiencing symptom improvement within hours of treatment. This immediate effect can provide much-needed respite, especially for those in crisis.
Effectiveness in Treatment-Resistant Cases
Ketamine stands out for its potential in treating treatment-resistant OCD. Many individuals who have tried SSRIs, CBT, or ERP without success report substantial improvement after ketamine therapy. While traditional treatments may offer partial relief or no relief at all for some, ketamine’s rapid action can be a game-changer for individuals who have exhausted other options.
Long-Term Results
While ketamine’s rapid effects are beneficial, long-term results tend to be more variable. The relief it provides is often short-lived, typically lasting days to weeks. This contrasts with SSRIs and CBT, which may take longer to produce noticeable results but can offer more sustained symptom management over time. For individuals who experience temporary relief from ketamine, repeated treatments may be necessary, making it more costly and time-consuming compared to conventional therapies.
Side Effects
Ketamine’s side effects, such as dissociation, elevated blood pressure, and nausea, are typically short-term but can be distressing for some patients. In contrast, SSRIs and CBT are generally well-tolerated, though SSRIs can have side effects like weight gain or sexual dysfunction. Ketamine’s potential for psychological dependence and the risks associated with frequent use are also concerns that don’t apply to traditional therapies.
Combination with Other Treatments
An advantage of ketamine is its ability to complement existing therapies. Integrating ketamine with CBT or ERP may provide a more holistic treatment plan, allowing individuals to benefit from the immediate relief ketamine offers while continuing to work on long-term behavioral change through therapy.
Conclusion
Ketamine represents a new frontier in the treatment of Obsessive-Compulsive Disorder, especially for those who have not responded to conventional therapies. Its ability to deliver rapid symptom relief offers hope to individuals with treatment-resistant OCD, providing a short-term reprieve from the intense cycle of obsessions and compulsions. While research has shown promising results, particularly in reducing symptoms within hours or days, these effects are often temporary, and long-term efficacy remains uncertain.
It’s important to remember that ketamine is not a cure, but rather a potential tool within a broader treatment plan. It should only be considered under the guidance of trained medical professionals, ideally in combination with ongoing therapy like CBT or ERP. As with any medical intervention, the risks and benefits must be carefully weighed.
For now, ketamine remains a promising but experimental option. As more large-scale studies emerge and guidelines are refined, it may eventually become a more widely accepted part of OCD treatment protocols. Until then, those considering ketamine should do so cautiously, staying informed and supported throughout their journey.
