Managing neuropathic pain, a complex and often debilitating condition can be challenging for both patients and healthcare providers. One emerging treatment that has garnered attention is the use of ketamine, a medication traditionally known for its anesthetic and dissociative properties.
This article delves into the nuances of neuropathic pain, the role of ketamine in its management, and the considerations and implications of this treatment approach. Let’s begin!
Table of Contents
Understanding Neuropathic Pain
Neuropathic pain is a chronic condition arising from damage to the nervous system, characterized by symptoms like burning, stabbing, and tingling sensations, and often includes hypersensitivity to stimuli. It can be caused by various conditions, such as diabetic neuropathy, postherpetic neuralgia, and spinal cord injuries.
The pain results from complex mechanisms, including nerve damage, central sensitization, and changes in brain chemistry. Diagnosing neuropathic pain is challenging due to its varied symptoms and overlap with other pain types.
It significantly impacts quality of life, leading to sleep disturbances, mood changes, and decreased mobility. Management typically involves a combination of medications, physical therapy, and psychological support tailored to the individual's specific needs.
Ketamine: An Overview
Ketamine, first synthesized in the 1960s, is a dissociative anesthetic with multiple medical applications. It primarily acts as an NMDA receptor antagonist, affecting pain, mood, and memory pathways.
While still used for anesthesia, particularly in emergency medicine, its sub-anesthetic doses are effective in managing chronic, especially neuropathic, pain and in treating resistant depression.
Ketamine can be administered in various forms, including intravenously and intranasally. Its use is regulated due to side effects like dissociation, hallucinations, and potential for abuse, necessitating careful medical supervision.
Despite these risks, ketamine is increasingly recognized for its therapeutic potential in pain management and mental health.

Mechanism of Action in Neuropathic Pain
Ketamine's mechanism of action in managing neuropathic pain involves several key aspects, primarily revolving around its role as an NMDA (N-methyl-D-aspartate) receptor antagonist. This mechanism is crucial for understanding how ketamine provides relief in neuropathic pain, a condition that can be resistant to conventional pain therapies.
NMDA Receptor Antagonism
Ketamine's primary mode of action in neuropathic pain is through its antagonistic effect on NMDA receptors. These receptors are critical in the transmission and modulation of pain signals in the nervous system.
When ketamine binds to these receptors, it inhibits their function, which disrupts the pain signaling pathways in both the spinal cord and brain. This inhibition is particularly effective in dampening the heightened pain response often seen in neuropathic pain conditions.
Additionally, by reducing the activity of glutamate, a key neurotransmitter that activates NMDA receptors, ketamine lessens the excitatory effects that contribute to pain perception.
Impact on Central Sensitization
Central sensitization is a phenomenon where the central nervous system becomes overly responsive to pain stimuli, a common feature in chronic neuropathic pain. Ketamine’s antagonism at the NMDA receptors plays a vital role in preventing or reversing this sensitization.
By modulating the pain signaling at the spinal and brain levels, ketamine can effectively decrease the hypersensitivity associated with neuropathic pain. This leads to a reduction in pain intensity and an improvement in overall pain management for patients suffering from chronic neuropathic conditions.
Additional Mechanisms
Beyond its role as an NMDA receptor antagonist, ketamine interacts with other receptors and neurotransmitter systems, contributing to its analgesic effects. It affects opioid receptors and monoaminergic pathways, which are also involved in pain perception and modulation.
These interactions further enhance ketamine’s ability to alleviate pain. Some studies also suggest that ketamine has anti-inflammatory effects, which could be beneficial in reducing pain that has an inflammatory component.
In summary, ketamine's effectiveness in treating neuropathic pain stems from its multifaceted mechanism of action, primarily as an NMDA receptor antagonist, but also through its interactions with other pain-related systems in the body. This makes it a unique and valuable tool in the management of neuropathic pain, offering relief where other treatments may fall short.
Clinical Evidence and Usage
Ketamine has shown promising results in managing neuropathic pain, particularly in cases where traditional treatments have failed. Clinical studies indicate its effectiveness in reducing pain in conditions like complex regional pain syndrome (CRPS) and fibromyalgia, often outperforming other pain medications.
Dosage and Administration
In clinical settings, ketamine is administered in various forms, including intravenous infusions, subcutaneous injections, nasal sprays, and oral compounds, with the dosage and method tailored to individual patient needs.
Its use requires careful monitoring due to potential side effects like dissociation, dizziness, nausea, and long-term risks such as cognitive impairment and bladder toxicity.
Ketamine therapy is generally considered for severe, refractory neuropathic pain, and its use in pain management is subject to regulatory oversight. The growing body of clinical evidence supporting its efficacy highlights ketamine's potential as a valuable option in neuropathic pain management.
Long-term outpatient use typically involves lower doses, either orally or through nasal sprays. Overall, ketamine's administration for neuropathic pain demands a personalized and cautious approach to ensure safety and effectiveness.
Potential Benefits
Ketamine's potential benefits in the management of neuropathic pain are multifaceted, offering hope to patients who have struggled with other treatments. Its unique pharmacological properties contribute to its effectiveness in various aspects of pain management.
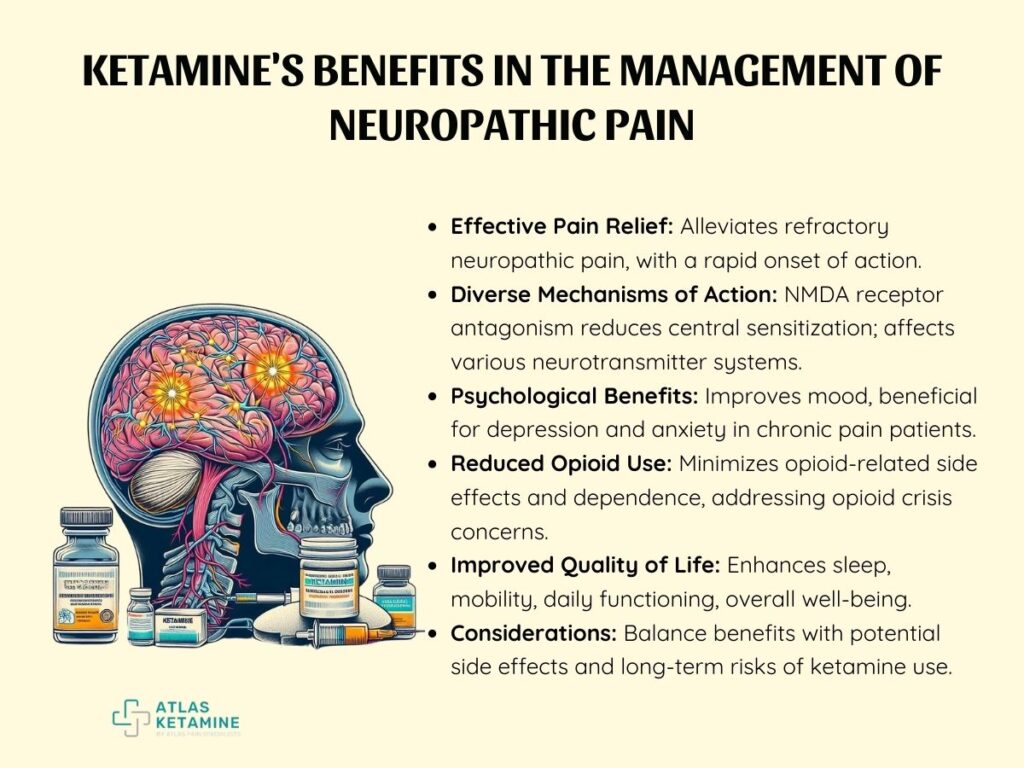
- Effective Pain Relief
Ketamine is particularly beneficial for patients with neuropathic pain that is resistant to conventional treatments. Unlike traditional analgesics, ketamine can effectively alleviate pain in cases where opioids, anticonvulsants, and antidepressants have failed, making it a critical option for those with refractory pain conditions.
Additionally, one of the key advantages of ketamine is its rapid onset of action, especially when administered intravenously. This quick relief is crucial for patients experiencing acute flare-ups of chronic neuropathic pain, providing swift and much-needed respite.
- Diverse Mechanisms of Action
The primary mechanism of ketamine in pain relief is NMDA receptor antagonism, which plays a significant role in reducing central sensitization, a common feature in neuropathic pain.
Furthermore, ketamine's influence extends to various neurotransmitter systems, allowing it to tackle different pain pathways. This broad spectrum of action enhances its effectiveness across a wide range of neuropathic pain syndromes, making it a versatile tool in pain management.
- Psychological Benefits
Beyond its physical analgesic effects, ketamine has shown the potential to improve psychological well-being. Patients with chronic pain often suffer from associated depression and anxiety, and ketamine's mood-enhancing properties can be particularly beneficial. This dual action on both pain and mood aspects can lead to a more holistic improvement in the overall health and well-being of patients.
- Reduced Opioid Use
In the context of the current opioid crisis, ketamine's ability to provide effective pain control and thereby reduce reliance on opioids is of significant importance. The opioid-sparing effect of ketamine not only minimizes the risk of opioid-related side effects but also addresses concerns related to tolerance and dependence associated with long-term opioid use.
- Improved Quality of Life
Effective management of neuropathic pain with ketamine can lead to substantial improvements in a patient's quality of life.
By controlling pain effectively, ketamine can enhance sleep quality, increase mobility, and improve daily functioning and well-being overall. This improvement in quality of life is a critical goal in the treatment of chronic pain conditions.
In conclusion, the potential benefits of ketamine in neuropathic pain management are diverse and significant. However, it's crucial to consider these benefits in the context of potential side effects and long-term risks associated with ketamine use.
Risks and Side Effects of Neuropathic Pain with Ketamine
The use of ketamine in managing neuropathic pain, while beneficial, is accompanied by several risks and side effects. These factors need careful consideration and management to ensure patient safety and the optimal use of ketamine as a therapeutic agent.
Psychotropic Effects
- Dissociative Experiences: One of the most notable side effects of ketamine is its dissociative properties, which can include feelings of detachment from reality, hallucinations, and altered perception. These effects are more pronounced at higher doses.
- Cognitive Impairment: There is a concern about the potential impact of ketamine on cognitive function, especially with prolonged use. This can manifest as memory impairment, reduced attention span, and difficulties in executive functioning.
Physical Side Effects
- Cardiovascular Effects: Ketamine can induce transient increases in blood pressure and heart rate, making it potentially risky for patients with underlying cardiovascular conditions.
- Nausea and Dizziness: These are common side effects, particularly soon after administration, and can affect a patient's ability to engage in daily activities.
Long-Term Risks
- Bladder Toxicity: Chronic use of ketamine has been associated with urinary tract symptoms and bladder toxicity, potentially leading to severe bladder problems.
- Dependency and Abuse Potential: Given its psychotropic effects, there is a risk of dependency and abuse with ketamine, especially when used outside of a controlled clinical setting.
Conclusion
Ketamine presents a promising, albeit complex, option in the arsenal against neuropathic pain. Its unique mechanism of action and potential efficacy in refractory cases make it a valuable tool for pain specialists.
However, careful patient selection, close monitoring, and a holistic approach to pain management are essential to maximize benefits and minimize risks. As research evolves, so will our understanding and utilization of ketamine in combating neuropathic pain.
